-
- Market Research
- |
- CBD Near Me
- |
- Giveaways
- |
- Newsletter
- |
- Contact
- |
- Advertise
- |

According to the CDC, roughly 20.4% of adults in the US experience some form of chronic pain and an additional 8% suffer from high-impact chronic pain. That’s nearly 70 million people and this does not include other common types of pain like acute and neuropathic. Understanding and identifying your type of pain in order to communicate with your healthcare provider can be a difficult task for some, but is a vital step towards getting relief.
Type of Pain: Table of Contents
Identifying Your Type of Pain
For many people, the term “pain” can be used to describe any type of bodily discomfort. However, not all types of pain are the same. Identifying the specific type of pain that you’re experiencing will help you get a head start in terms of locating the source and alleviating the discomfort.
Acute Pain
Based on a health education publication from the University of California Davis, acute pain is defined as a sensation that “begins suddenly and is usually sharp in quality.” Typically, acute pain is the type that most of us have experienced at some point. Acute pain is most commonly the result of a scuffed knee, minor burn, pulled muscle, or post-surgical discomfort.
By definition, acute pains are those that resolve themselves (or with medical intervention) within six months of the initial occurrence. Although this type of pain is common, you should always remain mindful of any type of pain that doesn’t resolve quickly as this is your body’s way of letting you know there’s an issue.
Chronic Pain
Chronic pain isn’t necessarily caused by a specific type of injury or issue but is simply a categorization of any pain that lingers for longer than six months. Chronic pains can stick around for years and even cause issues long after the original cause has healed. This type of pain almost always requires medical intervention as the body is not able to resolve the issue on its own.
Not only can chronic pain affect your day-to-day life in terms of mobility, but it can also take a toll on your mental health, leading to issues like depression or in extreme cases, suicidal ideation.
Nociceptive Pain
Nociceptive pain is undoubtedly the most frequent type of pain. The Beaumont Healthcare System described nociceptive pain as feeling “sharp, aching, or throbbing and is often caused by external injury like stubbing your toe.” Nociceptive pain can be classified as either acute or chronic depending on longevity.
Visceral Pain
Visceral pain, in a sense, is the opposite of nociceptive pain in terms of where it is felt. Visceral pain occurs internally and can be difficult to put a finger on the precise area where it is most intense. This type of pain feels like a “deep, squeezing, or colicky” sensation according to Holland-Frei’s Cancer Medication 6th edition.
In most cases, visceral pain is a signal that there are internal issues occurring. Conditions such as diverticulitis, IBS, and appendicitis are examples of conditions that typically result in visceral pain.
Somatic Pain
Somatic pain is classified as a pain that originates in your body’s tissues. This type of pain can be easily confused with visceral pain. One method to distinguish between somatic and visceral pain is how easily you can identify the epicenter or source of the pain. Visceral pain is often described as vague, while somatic pain is typically very easy to put a finger on the exact location where you’re experiencing the most discomfort.
Conditions that involve tissues (internal or external) like muscular damage, ligaments, tendons, or the skin are all areas that can be classified as somatic pain sources.
Neuropathic Pain
According to the National Institute of Neurological Disorders and Stroke, over 20 million Americans suffer from a form of neuropathic pain. This type of pain tends to be the most difficult for healthcare providers to pinpoint given the large number of variations and causes.
Neuropathic pain is a result of the body’s nerve receptors firing (and sometimes misfiring). It typically falls into the chronic categorization given how difficult it can be to diagnose and treat. Although researchers have not identified all sources of neuropathic pain, we do know that it is frequently a symptom experienced by, but not limited to chemotherapy, diabetes, HIV, spinal nerve damage, and CNS disorders.
Describing Your Type of Pain
Now that you have a better understanding of the various types of pain, there are a few other steps to take that can prove to be a valuable tool for your healthcare provider. Keeping a pain journal is highly recommended to identify trends that wouldn’t otherwise be noted.
Being that we live in the “there’s an app for everything” era, you have the option of keeping a traditional hand-written pain journal or utilizing one of the many pain journal apps available for most mobile devices.
Consistency is key when it comes to making the most of your pain journal. We recommend a daily log (at minimum) of the following topics:
- Time of Day: Does your pain occur during certain times of the day?
- Severity: Most healthcare providers utilize a 1-10 scale to describe pain severity.
- Location of Pain: Can you identify the area of your body where the pain occurs? Can you put your finger on the exact spot or does it occur in a generalized region of the body?
- Quantity: How often does the pain occur? How long does the pain typically last?
- Type: How would you describe your pain? Is it a piercing immediate pain or does it slowly intensify over time? This section will be vital to your healthcare provider in terms of identifying your type of pain.
- Cause: What causes your pain? Perhaps you notice it after going to the gym or after eating certain foods. Remember, you may not know what causes the pain, which is a completely acceptable answer as well.
- Treatment: Are there any medications or specific actions that alleviate the pain?
Can CBD Help Alleviate Pain?
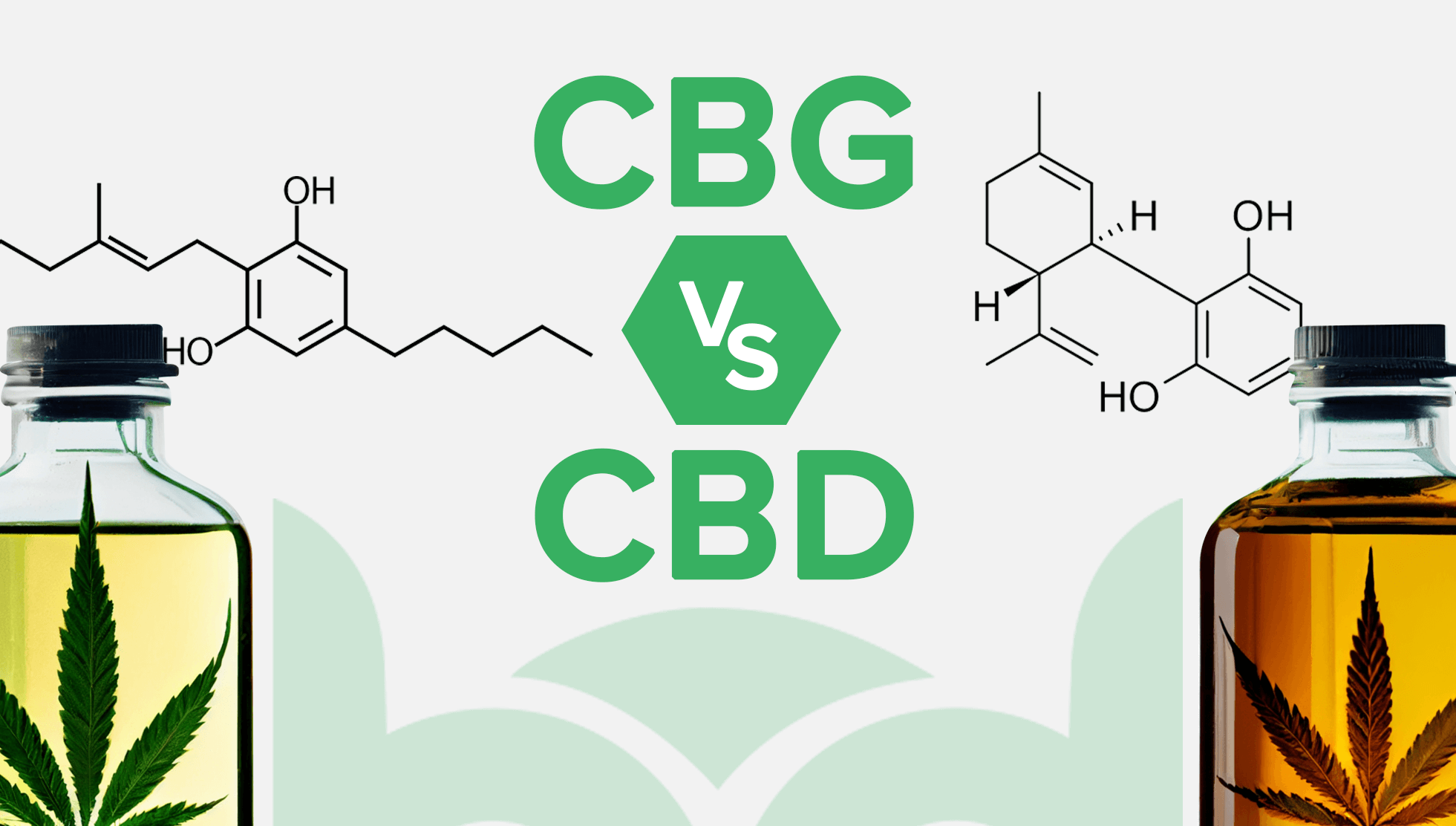
Possibly. Researchers around the world are conducting studies to determine CBD’s effectiveness in pain treatment.
A publication from the Journal of Pain Research studied the effects of a 12-week THC:CBD combination oral spray on participants who suffer from chronic pain. The data revealed that a 50% (and in some cases, more) pain reduction in those who received the THC:CBD solution compared to those who received placebos.
Of course, this doesn’t mean that CBD is the definitive answer to pain. Although early research and numerous anecdotal reports show promise that CBD may be capable of alleviating certain types of pain, most medical providers are awaiting additional clinical research results before forming their final opinion.
For the latest news and research data regarding CBD and its use in pain management, we recommend signing up for our free newsletter.
Conclusion
With its numerous classifications, trying to identify and treat pain can be an intimidating and disheartening task.
Accepting the concept that pain is simply our body trying to communicate with us is difficult, especially when it is occurring. As frustrating as it can be, oftentimes the first step to alleviating pain involves taking a deep breath, trying to relax, and attempting to decipher the message that your body is sending.
Medical technology is evolving faster than ever as well as our understanding of pain. Keeping a consistent pain journal to help clearly communicate symptoms to your medical provider is one of your best tools to not only determine the cause, but identifying your best treatment options as well.